Ways to Calm and Manage Colitis Flare Symptoms
Why Flares Happen and What This Guide Covers
Colitis flares can feel like a switch that flips without warning, but there are patterns, triggers, and tools you can use to regain control. A “flare” generally means your colon’s lining is inflamed and irritated, which often brings urgent bowel movements, diarrhea, rectal bleeding, cramping, and fatigue. In ulcerative colitis, this inflammation is limited to the colon and rectum, and it usually starts in the rectum before extending proximally. While no single strategy fits everyone, a practical plan—combining symptom relief, nutrition, medication adherence, and timely communication with your clinician—can shorten the rough patch and reduce complications. This guide aims to help you manage today’s flare and plan for calmer tomorrows, without quick fixes or unrealistic promises.
Here’s the roadmap you can expect as you read:
– What a flare is and why it matters: a clear, plain‑language overview with the most common triggers and warning signs.
– A 48‑hour action plan: hydration, diet adjustments, symptom tracking, and how to decide when to seek care.
– Ulcerative colitis–specific choices: when rectal therapies shine, how step‑up treatment works, and what “response” versus “remission” means.
– Food, fluids, and comfort strategies: low‑residue approaches during a flare, electrolyte tips, gentle movement, and skin care.
– Prevention and readiness: stress, sleep, vaccines, travel prep, and building a relapse‑resilient routine.
Flares deserve respect because they can escalate. Red flags include severe abdominal pain, high fever, signs of dehydration (dizziness, very dark urine, reduced urination), or significant continuous rectal bleeding. If these appear, contact your healthcare team promptly or seek urgent evaluation. Many people can start with at‑home steps while staying in touch with their clinician, especially for mild to moderate symptoms. Throughout the article, you’ll find comparisons—for example, soluble versus insoluble fiber, oral versus rectal treatments, and rest versus gentle activity—so you can choose what’s most suitable for your situation. Think of this as a field guide: evidence‑informed, practical, and focused on helping you move from uncertainty to a workable plan.
A 48‑Hour Flare Action Plan: Manage Colitis Flare Up
The first two days of a colitis flare set the tone. A calm, structured response can reduce symptom intensity and help you decide whether home care is enough or medical evaluation is needed. Start by simplifying your inputs and monitoring your outputs. Keep a short log noting bowel movements, visible blood, pain level, temperature, and fluids consumed. This is not busywork—patterns over 24–48 hours guide smarter choices and help your clinician if you need to check in.
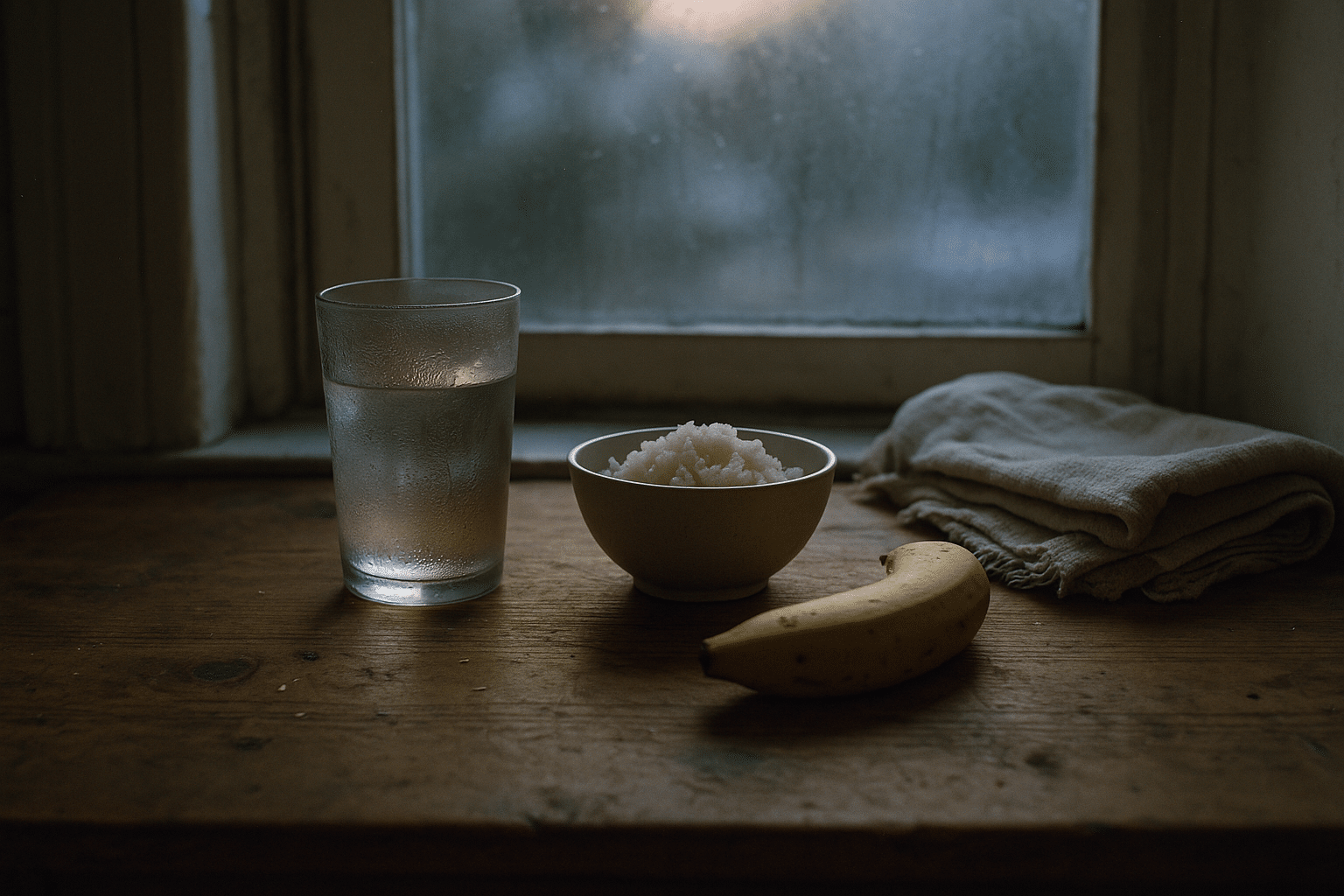
Hydration is foundational. Aim for frequent, small sips of water and add an oral rehydration approach with sodium and potassium if you have diarrhea. Practical cues include pale yellow urine and steady energy. Large gulps can worsen cramping, so think steady trickle, not flood. Nutrition during a flare should be gentle: consider a low‑residue, lower‑fat approach with small, frequent meals. Many find that refined grains (such as white rice or plain toast), bananas, applesauce, smooth nut butters (if tolerated), and tender proteins are easier than raw vegetables, seeds, or high‑fat dishes. If milk worsens symptoms, try lactose‑free options or limit dairy temporarily.
Medication adherence matters. Continue your maintenance therapy as prescribed; abruptly stopping controller medicines can backfire. For those already instructed by a clinician on how to step up therapy during a flare (for example, adding a topical rectal treatment or adjusting anti‑inflammatory dosing), follow that plan. Avoid non‑steroidal pain relievers unless your clinician has cleared them; they can aggravate the gut in some people. Over‑the‑counter anti‑diarrheals require caution—do not use them if you have high fever, severe pain, or significant bleeding, and always follow medical advice.
Comfort strategies help you stay functional. A warm compress or heating pad over the abdomen can soothe cramps. Gentle stretching or short walks may reduce gas discomfort without overtaxing you. Protect the skin: apply a barrier cream around the anus after cleaning with lukewarm water or fragrance‑free wipes to prevent irritation. Consider a brief, warm sitz bath after bowel movements.
Use a traffic‑light system for decisions: green for stable symptoms with mild urgency; yellow for increasing frequency, modest bleeding, or rising fatigue; red for persistent high fever, severe pain, dehydration, or heavy bleeding. If you enter the red zone—or if yellow persists beyond 48 hours—contact your healthcare team. Many regions report that inflammatory bowel disease affects millions of adults, and timely care helps prevent complications such as severe dehydration or hospitalization. This plan won’t eliminate the flare overnight, but it often steadies the ship while you line up further care if needed.
Ulcerative Colitis Flare Management: Choosing Paths That Fit
Ulcerative colitis (UC) flares follow a recognizable pattern: inflamed mucosa starting in the rectum and extending to a variable portion of the colon. Because of that anatomy, topical therapies that reach the rectum and left colon can be especially effective for many people with mild to moderate flares. A practical way to think about UC therapy is “local first, then systemic when needed,” always individualized with your clinician based on severity, location, and previous response.
For distal disease (proctitis or left‑sided colitis), rectal anti‑inflammatories—suppositories for rectal‑only involvement, enemas for left‑sided—can deliver medication directly to the inflamed lining, often with fewer whole‑body effects. Oral anti‑inflammatory agents may be used alone or combined with topical therapy to enhance coverage along the colon. For moderate to more severe flares, short courses of systemic corticosteroids may be considered under medical supervision to rapidly reduce inflammation; these can be potent but come with side‑effect considerations, so they’re generally used as a bridge rather than a long‑term solution.
When disease proves difficult to control or flares recur despite appropriate use of first‑line agents, your clinician may discuss advanced therapies—such as immunomodulators or targeted biologic and small‑molecule options—that address specific immune pathways. Two common strategies guide this decision: “step‑up,” where treatment intensity increases as needed, and “accelerated” or “top‑down” approaches in select situations where rapid control is important. The choice depends on severity, prior history, comorbidities, and personal preferences regarding monitoring and route of administration.
Objective markers can help track response. Many care teams use symptom scores alongside tests such as fecal calprotectin, C‑reactive protein, and endoscopic assessment to evaluate inflammation. It’s useful to distinguish symptom relief from mucosal healing: feeling better is the immediate goal during a flare, but reducing underlying inflammation lowers the chance of near‑term relapse. Discuss with your clinician how often to monitor, and what milestones define response, remission, and maintenance.
Practical tips enhance medical therapy: take medicines consistently, use correct rectal delivery techniques (for example, lying on the left side and remaining still for several minutes), and set reminders for multi‑dose regimens. Ask about vaccinations appropriate for people with immune‑mediated conditions, particularly before starting advanced therapies. Finally, partner early with your care team if symptoms escalate; studies consistently show that timely treatment of UC flares improves outcomes and reduces the likelihood of hospitalization. Think of UC flare management as a funnel: start with targeted local care when suitable, widen to systemic therapy when necessary, and use objective markers to keep you on course.
Reduce Colitis Flare Symptoms with Food, Fluids, and Comfort Strategies
Food and fluid choices won’t cure a flare, but they can noticeably soften the edges—less urgency, fewer cramps, and steadier energy. During a flare, the goal is to minimize mechanical and chemical irritation while maintaining hydration and sufficient calories. Many people do well with a low‑residue approach that reduces fiber bulk temporarily, then gradually reintroduces variety as symptoms improve. Practical ideas include white rice, pasta, plain crackers, soft eggs, tender poultry or tofu, clear broths, ripe bananas, and applesauce. If you tolerate it, smooth nut butters and strained soups offer calories without a lot of roughage. Avoid seeds, popcorn, raw cruciferous vegetables, spicy dishes, and greasy foods until your gut settles.
Fiber deserves nuance. Soluble fiber (oats, psyllium, ripe bananas) can form a gel that may help stool consistency, whereas insoluble fiber (wheat bran, raw greens, skins) can add abrasive bulk. During a flare, many find soluble fiber easier, while insoluble fiber is reintroduced later. Lactose can be a trigger for some; a brief lactose‑light trial is reasonable if you suspect sensitivity. Caffeine and alcohol can stimulate the gut; consider limiting them until symptoms recede.
Hydration is not just water. Diarrhea increases losses of sodium, potassium, and bicarbonate. An oral rehydration style drink—water, a pinch of salt, a source of glucose like diluted fruit juice, and a splash of citrus for taste—can help replace what you lose. Aim for small, frequent sips and monitor urine color as a real‑world indicator. If nausea is present, try chilled fluids, ice chips, or ginger tea; if vomiting persists or you cannot keep fluids down, seek medical advice promptly.
Comfort strategies round out the plan:
– Apply warmth to the abdomen to relax muscle spasm.
– Use a barrier cream after each bowel movement to protect skin.
– Try a brief sitz bath for soreness or spasm.
– Practice paced breathing: inhale for 4 counts, exhale for 6–8 counts during cramps.
– Take short, easy walks to reduce gas pooling.
Medication wise, adhere to your prescribed regimen and avoid adding non‑prescribed drugs without guidance. Over‑the‑counter anti‑diarrheals should be avoided in the presence of fever, severe pain, or significant bleeding. If hemorrhoids or fissures contribute to pain, gentle cleansing and topical protection can help while you address the underlying flare with your clinician. The theme is conservative, soothing care: keep inputs simple, protect the lining, replace losses, and give your body a predictable, calm environment in which to recover.
Preventing the Next Flare: Triggers, Stress, Sleep, and Travel Readiness
Prevention is not about perfection; it’s about stacking small advantages so the gut sees fewer surprises. Common trigger categories include infections, inconsistent medication use, certain pain relievers, smoking status changes, and high stress with inadequate sleep. Work with your clinician to keep vaccines up to date, especially if you use immune‑targeted therapies. If you need pain relief, ask about options that are gentler on the gut. Do not start or restart smoking to influence symptoms; the overall health risks outweigh any disease‑specific nuances.
Stress management is practical, not abstract. The brain‑gut axis is real—heightened stress can amplify gut motility and perceived pain. Choose two or three tools you will actually use: brief daily breathing exercises, a short mindfulness practice, or a simple journaling routine. Many people benefit from cognitive‑behavioral strategies that reframe catastrophic thinking during a flare. Gentle, regular physical activity—like walking or low‑impact strength work—supports sleep and mood, which in turn supports gut stability.
Sleep is a strong anti‑inflammatory ally. Aim for consistent bed and wake times, a cool dark room, and a wind‑down routine that nudges your nervous system toward rest. Reduce late‑evening meals and limit screen exposure in the hour before bed. If night‑time urgency disrupts rest, talk with your clinician about timing medications and fluids to minimize awakenings.
Build a relapse‑resilient routine:
– Set medication reminders and use a weekly pill organizer.
– Keep a simple symptom diary to spot trends early.
– Store a “flare kit” with barrier cream, soft wipes, a heating pad, and oral rehydration ingredients.
– Prepare a travel plan: aisle seats near restrooms, packing extra supplies, and carrying a written summary of your diagnosis and medications.
– Schedule periodic check‑ins to review labs or stool markers and align on goals.
Finally, cultivate a partnership mindset. Report changes early, especially new rectal bleeding, rising frequency, or weight loss. Ask about treatment targets that include both symptom control and reduction of measurable inflammation. Many adults live full, active lives with colitis; the aim is not to avoid every flare—an unrealistic goal—but to shorten, soften, and space them out while protecting long‑term health. With consistent habits, thoughtful medical care, and a ready plan, you can spend more time in the calm between storms.


